Through our partners at the Drug Development Solutions Center, we offer a Bile Acid-Dependent Hepatotoxicity study which provides an in vitro functional assay for assessment of your drug’s Cholestatic DILI risk. This patented assay, using sandwich-cultured primary human hepatocytes, is designed to determine whether a test article inhibiting the bile salt export pump (BSEP) causes bile acid accumulation leading to hepatocyte apoptosis. This effect could result in cholestatic drug-induced liver injury (DILI) and present risk to patients in clinical trials.

Bile Acid-Dependent Hepatotoxicity
You can now request quotes for our research services on BioIVT.com!
Whether you need a single assay or a complete ADME program, BioIVT’s experts will help design and implement the appropriate studies for your drug and research objectives. View BioIVT’s comprehensive portfolio of ADME research services.
Drug-induced liver injury (DILI) is characterized as liver injury due to intake of medications or xenobiotics, which leads to liver abnormalities or dysfunction [1]. DILI can also be referred to as drug induced hepatotoxicity.
There is a growing number of compounds that have been flagged for acute DILI risk and as a result been withdrawn from the market or are still on the market but issued with warnings [2,3], including:
- Ampicillin and other penicillin-based antibiotics
- Anabolic steroids
- Chlorpromazine
- Estradiol
- Imipramine
- Nitrofurantoin
- Oral contraceptives
- Prochlorperazine
- Sulindac
- Terbinafine
- Tolbutamide
- Bosentan
- Troglitazone (antidiabetic and anti-inflammatory)
- Nefazodone
- Cyclosporine
- Benzbromarone
- Sitaxsentan
The mechanism behind DILI is multifaceted and can be exacerbated by unpredictable metabolism and bodily response, as well as the complex relationship between an individual’s genetic makeup and environmental risk factors (4).
Furthermore, several factors may contribute to hepatocellular injury and cholestasis; including acute hepatocyte necrosis, the production of reactive metabolites (and oxidative stress) during cytochrome P450 (CYP) metabolism of the parent drug, activation of stress signaling, and mitochondrial dysfunction [5].
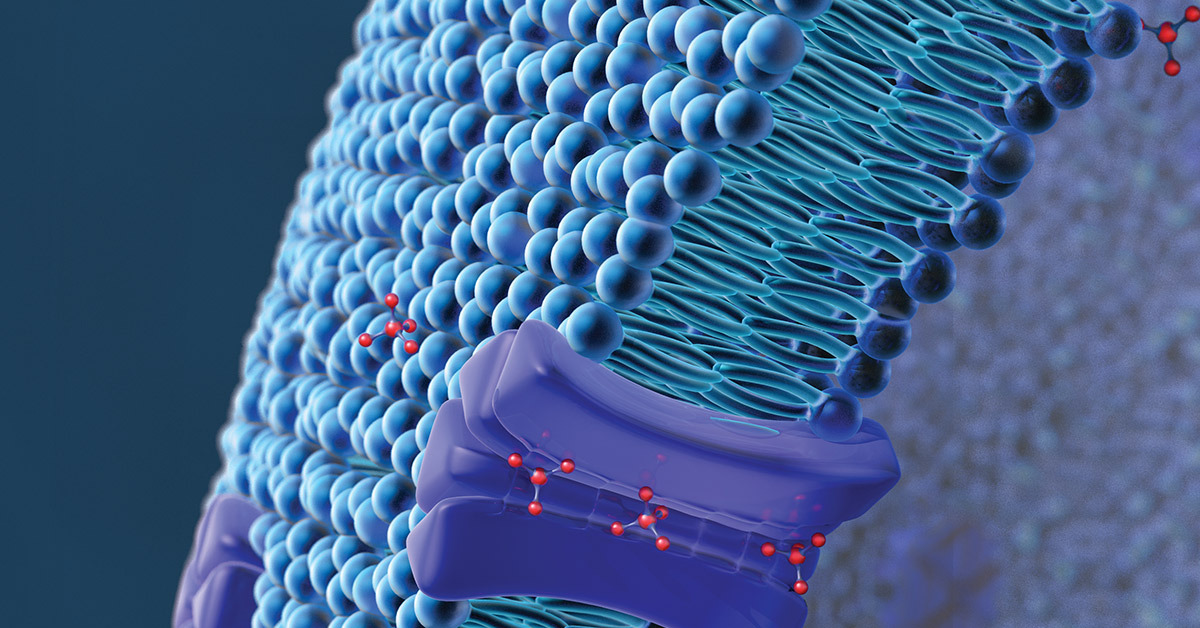
One postulated mechanism of DILI is cholestasis caused by inhibition of the bile salt efflux pump (BSEP), an ATP-binding cassette drug transporter mainly expressed in the canalicular membrane of hepatocytes where it facilitates excretion into the bile. When its function is disrupted, accumulation of bile acids can trigger apoptosis of hepatocytes leading to liver injury (cholestasis).
Proactive evaluation and understanding of BSEP inhibition is recommended in drug discovery and development to aid internal decision making on DILI risk.6
Hepatocytes may have some compensatory mechanisms in place to overcome BSEP inhibition, but using a predictive model to first answer the question “Can my investigational drug cause bile acid accumulation through BSEP inhibition?” can be a useful piece of information in toxicological assessment of risk.
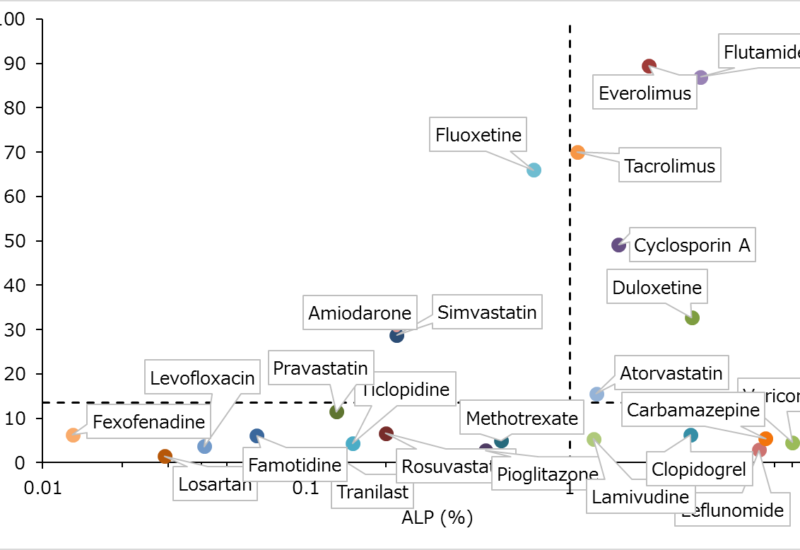
Our Bile Acid-Dependent Hepatotoxicity study is a functional assay which yields an IC50 value for your test article that can be used to assess bile acid-dependent cytotoxicity. Alternatively, you can use data from an abbreviated version of this study in our Receiver Operating Characteristics (ROC) Analysis, comparing in vitro results to other known cholestatic compounds to predict liver toxicity risk in human.
Bile Acid-Dependent Hepatotoxicity Assay Design
The Bile Acid-Dependent Hepatotoxicity study utilizes a patented technique licensed from Chiba University. This assay involves measuring lactate dehydrogenate (LDH) release from sandwich-cultured primary human hepatocytes incubated with the test drugs for 24 hours in the absence or presence of a bile acids mixture. If a test drug and/or its metabolite inhibits bile acid efflux from the hepatocytes, the accumulation of bile acids eventually induces cell death (apoptosis) which is detected by the release of LDH into medium.
Typical Study Timeline
- Day 1: Cell seeding with OptiCulture medium
- Day 2: Matrigel overlay
- Day 3: Medium change
- Day 4: Bile acid and drug exposure
- Day 5: Lactate dehydrogenase (LDH) measurement
Test System: Sandwich Cultured Hepatocytes (SCH)
In prerequisite in vitro assays, we can evaluate transporter inhibition potential using vesicles prepared from insect cells transiently transfected with a single efflux transporter or from mammalian cells chemically selected for the expression of a transporter. However, subcellular test systems lack the drug metabolism pathways and other bile acid efflux transporters that impact function in vivo and are important in evaluating complex cellular processes.
Sandwich-cultured hepatocytes (SCHs) present a “powerful in vitro tool” recommended to properly evaluate hepatobiliary drug transport [7]. Further, SCHs are metabolically competent and better represent functional bile networks than alternative test systems, making them a good model for evaluating biliary excretion of compounds and predicting cholestasis [8].
This assay uses XenoTech cryoplateable primary human hepatocytes from 1-3 donors in sandwich-culture. Our hepatocytes are regularly used in contracted in vitro assays at XenoTech and the Drug Development Solutions Center because they are trusted to deliver consistent, high-quality results in drug metabolism and drug transporter assays. Hepatocyte lots used for this hepatotoxicity study have been characterized for BSEP activity by scientists at the Drug Development Solutions Center.
The sandwich cultured hepatocytes are prepared in a 96-well plate with XenoTech OptiCulture media, Matrigel overlay, and a bile acid mixture to replicate in vivo conditions.
Bile Acids
To measure the response of human hepatocytes to influx of bile acids, the assay involves overlaying the sandwich culture with a representative bile acid mixture in addition to culture medium and Matrigel overlay. The mixture includes:
- Cholic acid
- Chenodeoxycholic acid
- Ursodeoxycholic acid
- Lithocholic acid
- Taurocholic acid
- Taurochenodeoxycholic acid
- Tauroursosdeoxycholic acid
- Taurolithocholic acid
- Glycocholic acid
- Glycodeoxycholic acid
- Glycochenodeoxycholic acid
- Deoxycholic acid
LDH Measurement
For this study, cytotoxicity will be assessed by the amount of lactate dehydrogenase (LDH) released into the culture media. Culture medium-associated LDH activity will be measured using a commercially available cytotoxicity assay kit. Hepatocytes treated with cytotoxic positive control is used to establish a toxicity threshold to which the test article-treated culture can be compared.
Report Deliverables to Assess Cytotoxicity
At completion of an in vitro Bile Acid-Dependent Hepatotoxicity study, you will receive a report containing these key results:
- Cytotoxicity ratio
- EC50 (µmol/L)
- EC50 ratio
Cytotoxicity Ratio
This ratio compares percentage of cytotoxicity in cultures with and without bile acid mixture. Percentage of toxicity is calculated using values of mean absorbance of solvent control, cytotoxicity positive control, and test article-treated culture.
Percentage of cytotoxicity (%) = (S − N) / (P − N) × 100
S: Mean absorbance of each samples in three wells
N: Mean absorbance of solvent control in three wells
P: Mean absorbance of cytotoxicity positive control in three wells
EC50
If pre-established cytotoxicity criteria are met, indicating the test article does elicit a cholestatic effect, then EC50 values for cultures with and without bile acid mixture will be provided along with an EC50 ratio comparing the two.
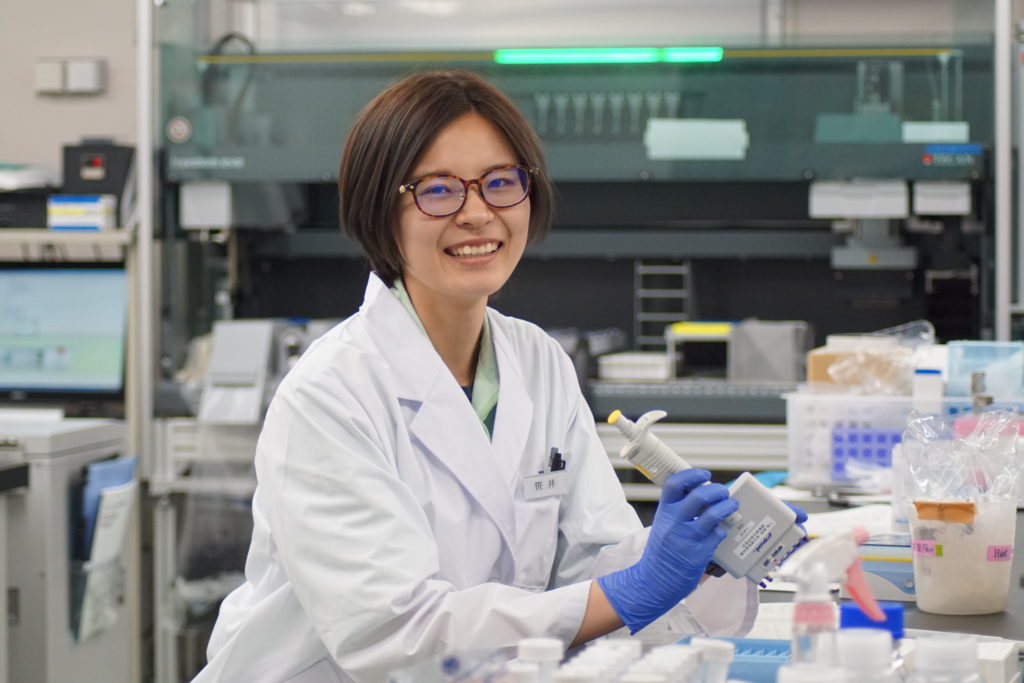
To learn more about the way this study is designed and executed, watch our webinar, “In Vitro Cholestatic DILI & Mitochondrial Toxicity Studies to Assess Hepatotoxicity” presented by Miki Fujishima from the Drug Development Solutions Center.
References
- Suk, Ki Tae, and Dong Joon Kim. “Drug-Induced Liver Injury: Present and Future.” Clinical and molecular hepatology 18.3 (2012): 249–257. PMC. Web. 24 Mar. 2015.
- Morgan, R.E., Trauner, M., van Staden, C.J., Lee, P.H., Ramachandran, B., Eschenberg, M., Afshari, C.A., Qualls, C.W., Lightfoot-Dunn, R., Hamadeh, H.K., “Interference with Bile Salt Export Pump Function is a Susceptibility Factor for Human Liver Injury in Drug Development.” Toxicol. Sci., (2010) 118, (2), 485-500.
- “Drug-Induced Cholestasis.” UF Health, University of Florida Health, 23 May 2012, ufhealth.org/drug-induced-cholestasis.
- Chen, M., Bisgin, H., Tong, L., Fang, H., Borlak, J., Tong, W., “Toward predictive models for drug-induced liver injury in humans: are we there yet?” (2014) Biomarkers Med., 8 (2), 201-213.
- Yuan L, Kaplowitz N. “Mechanisms of Drug Induced Liver Injury.” Clinics in liver disease. 2013;17(4):507- 518.
- Swift, Brandon, et al. “Sandwich-Cultured Hepatocytes: Anin Vitromodel to Evaluate Hepatobiliary Transporter-Based Drug Interactions and Hepatotoxicity.” Drug Metabolism Reviews, vol. 42, no. 3, 2010, pp. 446–471., doi:10.3109/03602530903491881.
- Yang, Kyunghee, et al. “Sandwich-Cultured Hepatocytes as a Tool to Study Drug Disposition and Drug-Induced Liver Injury.” Journal of Pharmaceutical Sciences, vol. 105, no. 2, 2016, pp. 443–459., doi:10.1016/j.xphs.2015.11.008.
- Aleo, Michael D., et al. “Human Drug-Induced Liver Injury Severity Is Highly Associated with Dual Inhibition of Liver Mitochondrial Function and Bile Salt Export Pump.” Hepatology, vol. 60, no. 3, 2014, pp. 1015–1022., doi:10.1002/hep.27206.